Discover the Healing Power of Movement
Physiotherapy promotes recovery and enhances mobility.
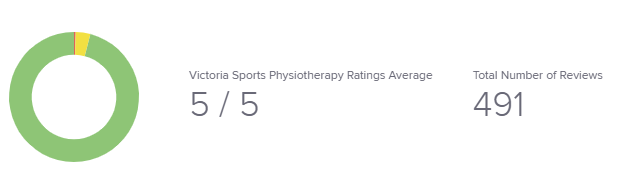
What our patients are saying in the clinic, with JANE Reviews
Rediscover your freedom of movement
Schedule your physiotherapy session in Prince George today and start feeling better
ContactWhat We Treat
Musculocutaneous Injuries
Arthritis is an umbrella term for a group of conditions characterized by inflammation and/or degeneration of one or more joints, leading to pain, stiffness, swelling, reduced range of motion, and functional limitation. It is not a single disease, but a category that includes over 100 different joint disorders with distinct causes and mechanisms.
Back Pain: Strain or Sprain
A back strain or sprain is an acute or subacute musculoskeletal injury involving excessive tensile or shear loading of the soft tissues of the spine, resulting in microscopic or macroscopic damage to muscles and tendons (strain) and/or ligaments and joint capsules (sprain), leading to localized pain, muscle spasm, stiffness, and temporary limitation of spinal movement without structural damage to the vertebrae or intervertebral discs.
-
Strain: Injury to muscle or tendon fibers of the back
-
Sprain: Injury to ligaments or joint capsules that stabilize the spinal segments
These injuries most commonly affect the lumbar (low back) region, but can also occur in the thoracic or cervical spine.
Back Pain: Sciatica
Sciatica is a symptom complex characterized by pain radiating from the lower back or buttock down the posterior or lateral aspect of the leg, caused by irritation or compression of one or more lumbosacral nerve roots (most commonly L4–S1). It may be accompanied by numbness, tingling, or muscle weakness in the affected nerve distribution.
Back Pain: Bulging Disc (Disc Protrusion)
A bulging disc refers to circumferential, symmetric extension of the intervertebral disc beyond the margins of the vertebral bodies, due to degeneration or mechanical stress, without focal rupture of the outer annulus fibrosus. It may or may not compress nearby nerve roots and is often asymptomatic.
Chronic pain is pain that persists or recurs for longer than the normal expected time of tissue healing, typically defined as lasting more than 3 months, and is associated with ongoing biological, psychological, and social factors that may maintain or amplify the pain experience, even in the absence of ongoing tissue damage.
Neck pain is an unpleasant sensory experience arising from actual or potential tissue injury or dysfunction in the cervical spine and surrounding structures, including muscles, ligaments, intervertebral discs, facet joints, and neural tissues, resulting in pain, stiffness, and/or reduced movement in the neck region, with or without radiation into the head, shoulders, or upper limbs.
Shoulder pain is an unpleasant sensory experience arising from actual or potential tissue injury or dysfunction of the structures of the shoulder complex, including the glenohumeral joint, acromioclavicular joint, scapulothoracic articulation, rotator cuff tendons, bursae, ligaments, capsule, and surrounding muscles, resulting in pain, stiffness, weakness, and/or restricted upper-limb movement, with possible radiation into the upper arm or neck.
Elbow pain is an unpleasant sensory experience arising from actual or potential tissue injury or dysfunction of the structures of the elbow region, including the humeroulnar, humeroradial, and proximal radioulnar joints, surrounding ligaments, tendons, muscles, bursae, and neural tissues, resulting in pain, tenderness, stiffness, weakness, and/or limitation of arm and hand function.
Wrist pain is an unpleasant sensory experience arising from actual or potential tissue injury or dysfunction of the structures of the wrist complex, including the radiocarpal and midcarpal joints, carpal bones, intercarpal ligaments, triangular fibrocartilage complex (TFCC), tendons, tendon sheaths, bursae, and peripheral nerves, resulting in pain, stiffness, weakness, instability, and/or limitation of hand and forearm function.
Hand pain is an unpleasant sensory experience arising from actual or potential tissue injury or dysfunction of the structures of the hand, including the metacarpophalangeal (MCP), proximal and distal interphalangeal (PIP, DIP) joints, phalanges, intrinsic and extrinsic muscles, tendons and tendon sheaths, ligaments, fascia, vascular tissues, and peripheral nerves, resulting in pain, stiffness, swelling, weakness, altered sensation, and/or impaired fine motor function.
Hip pain is an unpleasant sensory experience arising from actual or potential tissue injury or dysfunction of the structures of the hip region, including the femoroacetabular joint, acetabular labrum, articular cartilage, joint capsule, surrounding ligaments, muscles, tendons, bursae, and nearby neural or vascular structures, resulting in pain, stiffness, weakness, and/or limitation of lower-limb and trunk function.
Knee pain is an unpleasant sensory experience arising from actual or potential tissue injury or dysfunction of the structures of the knee joint and surrounding region, including the tibiofemoral and patellofemoral joints, menisci, articular cartilage, ligaments, joint capsule, synovium, muscles, tendons, and bursae, resulting in pain, stiffness, swelling, instability, weakness, and/or limitation of lower-limb function.
Ankle and foot pain is an unpleasant sensory experience arising from actual or potential tissue injury or dysfunction of the structures of the ankle and foot, including the talocrural and subtalar joints, midfoot and forefoot joints, bones, articular cartilage, ligaments, plantar fascia, muscles, tendons, bursae, and peripheral nerves, resulting in pain, swelling, stiffness, weakness, altered gait, and/or limitation of weight-bearing and balance activities.
Muscle, tendon, or ligament injuries are acute or subacute musculoskeletal injuries characterized by excessive tensile loading that exceeds the tissue’s capacity, resulting in microscopic or macroscopic disruption of fibers, local inflammation, pain, swelling, reduced strength or stability, and impaired movement or function.
They are classified by tissue type and mechanism:
-
Strain: An injury to muscle or tendon fibers caused by overstretching or excessive contraction, often occurring during rapid acceleration, deceleration, or heavy loading.
-
Sprain: An injury to ligament fibers caused by excessive joint movement beyond normal physiological limits, leading to partial or complete tearing of stabilizing structures.
Severity is commonly graded:
-
Grade I: Mild fiber disruption, minimal strength loss
-
Grade II: Partial tear, moderate pain and functional limitation
-
Grade III: Complete rupture, significant instability or loss of function
Tendinitis (Tendonitis)
Tendinitis is an acute inflammatory condition of a tendon characterized by pain, swelling, warmth, and impaired function, typically occurring shortly after sudden or excessive loading. It reflects a short-term inflammatory response and is relatively uncommon in chronic tendon pain.
Key features:
-
True inflammation present
-
Usually short-term and reactive
-
Often follows sudden overload or trauma
Tendinopathy
Tendinopathy is a chronic tendon disorder characterized by tendon pain, thickening, and impaired load tolerance associated with degenerative changes in tendon structure, altered collagen organization, and minimal or absent inflammation. It represents a failed or dysregulated healing response to repeated mechanical loading.
Key features:
-
Degenerative and structural changes, not classic inflammation
-
Often chronic and recurrent
-
Pain related to load and activity
-
Includes subtypes such as:
-
Reactive tendinopathy
-
Tendon disrepair
-
Degenerative tendinopathy (continuum model)
-
Bursitis is an inflammatory condition of a bursa, characterized by increased synovial fluid production, bursal wall thickening, and localized pain, swelling, and tenderness, resulting from mechanical irritation, repetitive friction, direct trauma, infection, or systemic inflammatory disease.
A bursa is a small, fluid-filled sac located between tissues (such as tendon and bone or skin and bone) that reduces friction and allows smooth movement.
Orthopedics is the medical specialty concerned with the prevention, diagnosis, treatment, and rehabilitation of disorders, injuries, and diseases of the musculoskeletal system, including bones, joints, muscles, tendons, ligaments, cartilage, and related neurovascular structures, using both surgical and non-surgical approaches to restore function, reduce pain, and improve quality of life.
Orthopedic care spans:
-
Traumatic injuries (fractures, dislocations, ligament tears)
-
Degenerative conditions (osteoarthritis, spinal degeneration)
-
Congenital and developmental disorders (scoliosis, hip dysplasia)
-
Overuse and sports injuries
-
Post-surgical rehabilitation and long-term functional recovery
Pre- and post-surgery rehabilitation refers to a structured, evidence-based program of assessment, education, and therapeutic interventions delivered before and after a surgical procedure, designed to optimize physical and psychological readiness for surgery, enhance tissue healing, restore function, prevent complications, and promote safe return to daily activities, work, and sport.
It includes two complementary phases:
Pre-Surgery Rehabilitation (Prehabilitation)
Prehabilitation is the process of improving a patient’s physical capacity, movement quality, and health behaviors prior to surgery in order to improve surgical outcomes and accelerate post-operative recovery.
Goals include:
-
Improving strength, mobility, and cardiovascular fitness
-
Educating the patient on post-op expectations and exercises
-
Reducing pain, inflammation, and fear of movement
-
Optimizing comorbidities and lifestyle factors (sleep, activity)
Post-Surgery Rehabilitation
Post-surgery rehabilitation is the progressive restoration of movement, strength, neuromuscular control, and functional capacity following surgical intervention, while respecting tissue healing timelines and surgical precautions.
Goals include:
-
Protecting surgical repair and supporting healing
-
Restoring range of motion and strength
-
Re-training movement and load tolerance
-
Preventing complications (stiffness, weakness, falls, re-injury)
-
Returning to work, sport, and independent living
The temporomandibular joint (TMJ) is the paired synovial joint connecting the mandible (lower jaw) to the temporal bone of the skull, allowing complex movements required for chewing, speaking, and yawning, including hinge (rotation) and sliding (translation) motions.
TMJ disorders (collectively termed Temporomandibular Disorders, or TMD) are a group of musculoskeletal and neuromuscular conditions affecting the temporomandibular joint, the articular disc, and the surrounding masticatory muscles, characterized by jaw pain, joint noises, restricted or asymmetric jaw movement, and sometimes associated head, neck, or ear symptoms.
Vertigo
Specific type of dizziness characterized by a false sensation of movement, most commonly a spinning or rotational feeling, occurring when there is asymmetrical or inappropriate signaling within the vestibular system or its central nervous system connections, leading the brain to incorrectly perceive motion.
Vertigo arises from dysfunction in:
-
The peripheral vestibular system (inner ear structures), or
-
The central vestibular pathways (brainstem and cerebellum)
It is commonly accompanied by:
-
Nystagmus (involuntary rhythmic eye movements)
-
Nausea or vomiting
-
Postural instability
Benign Paroxysmal Positional Vertigo (BPPV) is a vestibular disorder caused by the displacement of otoconia (calcium carbonate crystals) from the utricle into one of the semicircular canals of the inner ear, resulting in brief episodes of Vertigo (See Definition Above) triggered by specific changes in head position relative to gravity.
Balance is the ability to maintain the body’s center of mass within the base of support during static and dynamic activities through the coordinated integration of sensory input (visual, vestibular, and somatosensory systems), central nervous system processing, and appropriate motor responses to control posture and movement.
Dizziness is a non-specific term describing a subjective sensation of disturbed spatial orientation, which may include feelings of lightheadedness, unsteadiness, imbalance, or a sensation of movement, arising from dysfunction in the vestibular system, visual system, somatosensory system, cardiovascular system, or central nervous system integration of these inputs.
headache is an unpleasant sensory experience characterized by pain perceived in the head, face, or upper neck, arising from activation or sensitization of pain-sensitive structures such as blood vessels, meninges, cranial and cervical nerves, muscles, and connective tissues, and influenced by central nervous system pain processing.
Running Assessments
Pain experienced during running is a musculoskeletal or neuromuscular symptom arising from repetitive mechanical loading that exceeds the adaptive capacity of tissues involved in running, including muscles, tendons, bones, joints, fascia, and peripheral nerves, resulting in localized or regional pain that is typically activity-related and load-dependent.
This pain reflects a mismatch between tissue load and tissue capacity, rather than a single traumatic event, and may involve:
-
Muscle overload or fatigue (e.g., delayed onset muscle soreness, strains)
-
Tendon disorders (tendinopathy) due to repetitive tensile loading
-
Bone stress reactions or stress fractures from cumulative impact
-
Joint irritation or cartilage overload
-
Fascial or compartment-related pain
-
Neural irritation in less common cases
Running performance is the capacity to run at a given speed, distance, or intensity with efficiency, consistency, and minimal fatigue or injury risk, determined by the integrated function of cardiovascular fitness, neuromuscular strength and coordination, biomechanical efficiency, metabolic capacity, and psychological factors.
It reflects not only how fast or far a person can run, but how effectively the body converts physiological and mechanical resources into forward motion over time.
How We Treat
Exercise prescription is the systematic, individualized planning and delivery of physical activity and therapeutic exercise based on assessment of a person’s health status, functional capacity, goals, and risk factors, using specific parameters of type, intensity, frequency, duration, and progression to achieve targeted physiological and functional outcomes safely and effectively.
It is a core component of rehabilitation, injury prevention, chronic disease management, and performance enhancement.
Exercise prescription is guided by the FITT-VP principles:
-
Frequency
-
Intensity
-
Time (duration)
-
Type (mode of exercise)
-
Volume (total load)
-
Progression (planned increases over time)
Manual therapy is a group of skilled, hands-on techniques applied by a trained clinician to the muscles, joints, connective tissues, and neural structures with the aim of reducing pain, improving mobility, modulating nervous system sensitivity, and facilitating movement and function as part of a comprehensive rehabilitation or treatment program.
Manual therapy techniques may include:
-
Joint mobilization and manipulation
-
Soft tissue mobilization
-
Myofascial techniques
-
Neural mobilization
-
Passive stretching and traction techniques
Manual therapy is most effective when used to support and enable active rehabilitation, rather than as a stand-alone treatment.
Dry needling is a skilled therapeutic technique in which a trained clinician inserts thin, solid filiform needles into muscle tissue, myofascial trigger points, or other soft tissues with the aim of reducing pain, decreasing neuromuscular irritability, improving local blood flow, and facilitating restoration of normal movement and function.
The term “dry” indicates that no medication or injection is delivered through the needle, distinguishing it from injections such as corticosteroids or anesthetics.
Dry needling is based on modern neurophysiological and musculoskeletal principles and may target:
-
Myofascial trigger points
-
Taut muscle bands
-
Connective tissue interfaces
-
Peri-neural tissues (with caution and training)
Vestibular therapy is a specialized, exercise-based rehabilitation approach designed to reduce dizziness, vertigo, gaze instability, and balance impairments by promoting central nervous system compensation for dysfunction of the vestibular system through targeted adaptation, habituation, and substitution strategies.
It is used to treat conditions affecting:
-
The inner ear balance organs (peripheral vestibular system), and/or
-
The central nervous system pathways that process balance and spatial orientation.
Vestibular therapy programs are individualized and may include:
-
Gaze stabilization exercises (to improve visual clarity during head movement)
-
Habituation exercises (to reduce symptoms triggered by specific movements)
-
Balance and gait training
-
Canalith repositioning maneuvers (for BPPV, such as the Epley or BBQ roll)
Gait and running analysis is the systematic assessment of walking or running mechanics through observation and/or instrumented measurement of movement patterns, joint kinematics, muscle activation, and loading forces, with the aim of identifying biomechanical factors that contribute to injury risk, pain, movement inefficiency, or performance limitations, and to guide targeted rehabilitation or performance interventions.
It evaluates how the body:
-
Moves through each phase of stance and swing
-
Absorbs and generates forces
-
Coordinates joints and muscles across the kinetic chain
Traction is a therapeutic technique that applies a controlled, longitudinal pulling force to the spine or a limb with the aim of reducing compressive forces on joints and soft tissues, increasing joint space, decreasing pain, and temporarily improving mobility by stretching muscles, ligaments, and joint capsules and modulating neural sensitivity.
In musculoskeletal and rehabilitation settings, traction is commonly applied to:
-
The cervical spine (neck)
-
The lumbar spine (low back)
-
Less commonly, to peripheral joints
Traction may be delivered as:
-
Manual traction — applied by a clinician using their hands
-
Mechanical traction — using devices that apply adjustable force
-
Static traction — sustained pull
-
Intermittent traction — cycles of pull and release
he Graston Technique is a form of instrument-assisted soft tissue mobilization (IASTM) that uses specially designed stainless-steel instruments to apply controlled mechanical stress to muscles, tendons, fascia, and connective tissues, with the aim of reducing pain, improving tissue mobility, promoting remodeling of dysfunctional soft tissue, and facilitating improved movement and function.
The technique is based on the principle that repetitive loading and micro-stimulation of soft tissues can stimulate a localized healing response, improve tissue extensibility, and modulate pain, while also allowing the clinician to better detect areas of tissue restriction or sensitivity.
Graston is typically used as part of a broader rehabilitation program that includes:
-
Therapeutic exercise
-
Mobility work
-
Movement retraining
-
Load progression
Therapeutic taping is the clinical application of adhesive tape to the skin using specific techniques intended to provide mechanical support, influence joint or soft tissue positioning, modify movement patterns, reduce pain, and enhance proprioceptive feedback, as an adjunct to rehabilitation and functional activity.
Different taping methods are selected based on the therapeutic goal and tissue involved, and may target:
-
Joint stabilization or unloading
-
Muscle facilitation or inhibition
-
Edema management
-
Postural or movement cueing
Common categories include:
-
Rigid athletic taping (for mechanical support and injury protection)
-
Elastic therapeutic taping (e.g., kinesiology tape) (for sensorimotor and movement effects)
Therapeutic cupping is a manual therapy technique in which negative pressure is created inside cups placed on the skin to lift superficial tissues, with the aim of increasing local blood flow, altering connective tissue mobility, modulating pain through neurophysiological mechanisms, and facilitating movement as part of a broader rehabilitation or recovery program.
The cupping technique that we employ is:
-
Dynamically (moving cupping), where cups are glided over tissues after applying lubricant.
Orthotics are externally applied medical devices designed to support, align, prevent, or correct deformities, improve biomechanical function, redistribute forces, and reduce pain by modifying the way loads are transmitted through the body during standing and movement.
They are most commonly used in footwear as foot orthoses, but may also include devices for other body regions (e.g., ankle-foot orthoses, knee braces, spinal orthoses).
Our Orthotics are:
-
Custom-made, based on individual assessment and foot morphology
Rediscover your freedom of movement
Victoria Sports Physiotherapy
108-1669 Victoria Street.,Prince George, BC
V2L 2L5 View Staff & Treatments



.png)
.jfif)

.png)
